4 Major Factors to Prevent Heat-Related Illness and Fatalities

Experts in the athletic field have long studied the impact heat stress can have on athletes of all ages and levels. What can safety managers learn by applying these findings to industrial settings?
In August of 2001, NFL player Korey Stringer tragically died as a result of heat stroke complications brought on during Minnesota Vikings’ training camp. The heartbreaking incident shed light on the detrimentally overlooked risk of extreme heat—one that, despite being entirely preventable, results in over 700 deaths per year according to the CDC.
Since Stringer’s death, the Korey Stringer Institute (started by his wife Kelci and exertional heat stroke expert Douglas Casa) has made it their mission to “provide research, education, advocacy and consultation to maximize performance, optimize safety and prevent sudden death for the athlete, warfighter and laborer.”
The institute’s work includes the identification of four factors in eliminating heat-related illness and fatalities: Hydration, Heat Acclimatization, Work-to-Rest Ratio and Body Cooling Throughout the Shift.
But before we break those down, humor us as we go Bill Nye on the situation and hit you with a little science behind the risk…
IT’S ALL THERMOREGULATION, BABY
Thermoregulation is a catch-all term for the various processes the body uses to maintain its internal temperature. Things like shivering when it’s cold or sweating when it’s hot.
How does sweating help with thermoregulation?
To reduce heat, blood vessels widen to allow heat energy to radiate out of the skin’s surface—a.k.a., sweating. As sweat evaporates off the skin, it naturally cools the body.
When exposed to extreme heat for too long, the body can’t sustain that normal cooling process—resulting in hyperthermia. If temperature can be cooled within 30 minutes, studies show there is a 100% survival rate. But if the body goes into prolonged hyperthermia, life-altering heat-related illness such as heat stroke can occur.
WHO’S MOST AT RISK FOR HEAT-RELATED ILLNESS?
While construction crews certainly take the brunt of the burn, a wide variety of industries pose a serious heat stress risk for workers both indoors and out. The following is a list of those who have actively participated in OSHA’s Heat Illness Prevention Campaign to educate employers and crews on the dangers of working in the heat.
- Outdoor: Construction, logging, landscaping, agriculture, postal/delivery, fisheries, wildland firefighting, maritime, utilities, railroads, EMTs, oil & gas, sanitation
- Indoor: Warehousing, food processing, foundries, manufacturing, mills, automotive

Now that you know what and who we’re dealing with, let’s get to what you really came for—the solutions.
HEAT STRESS PREVENTION FACTOR 1:
HYDRATION
This is the big ‘un. Water accounts for 60% of body weight, 75% of muscles and 80% of the brain. It is, literally, the foundation for all life.
When exposed to extreme heat for too long, sweat production increases in order to more rapidly cool down the body. This process itself is a good thing. Where it becomes an issue is when the water and salt lost through excess sweating isn’t being replaced quickly enough to sustain the thermoregulation process—inducing dehydration and putting workers on a fast track to heat-related illness.
OSHA recommends workers gradually replace lost fluids with 5-7oz of water every 20 minutes. For jobs lasting longer than two hours, electrolyte beverages should also be provided to help workers replace the salt (a.k.a. electrolytes) being lost through sweat. Because salt retains water, keeping levels constant is critical to proper hydration.
Unlike athletics where water is often readily available, it’s important for safety managers to consider that working in the heat comes with its own logistical challenges to keep crews chugging. Many worksites are relatively remote (think underground or at-heights) which can make it much harder to continuously supply cool fresh water. Beyond that, workers are often wearing heavy PPE that can be a hassle to remove every time they need to take a sip.

While diligent monitoring of potable water supplies and distribution of on-the-go solutions such as hydration packs are a critical piece of the puzzle, it’s equally important for safety managers to hammer home the importance of water intake and educate workers on how to recognize symptoms of dehydration.
Reactions such as muscle cramps and dizziness are pretty obvious signs but many don’t realize that, by the time that first inkling of thirst sets in, the body is already dehydrated. So how do you monitor fluid intake before it’s too late? It’s actually quite easy—study the stream. The darker your urine, the more severe your dehydration. Don’t overdo it though… a totally clear stream is an indication of overhydration, which is an entirely other issue in itself.

Download hydration jobsite poster >>>
HEAT STRESS PREVENTION FACTOR 2:
ACCLIMATIZATION TO HEAT
Even though almost 70% of heat-related illnesses occur within the first few days of extreme heat, acclimatization remains one of the most frequently overlooked, misunderstood and mispronounced prevention tactics (seriously though, we feel like Nemo struggling to pronounce “anemone”—which, if you think you’re too tough to watch Finding Nemo... you’re dead wrong).
The California Heat Illness Prevention Standard (the most substantial set of regulations you’ll find in the US) defines acclimatization as the “temporary adaptation of the body to work in the heat that occurs gradually when a person is exposed to it.” This process is of course important for new workers, but equally so for those in regions prone to unexpected heat waves. The same reason you wouldn’t cannonball into a hot tub, acclimatization allows your body to safely ease in over the course of a few days to a few weeks.

How long does acclimatization to heat take?
Acclimatization generally requires between 7-14 days depending on the extremity of heat in the environment. During the first few days of acclimatization, core temperature and heart rate will be at their highest. Over time, this physical strain will decrease—dramatically improving comfort and overall functioning. Successful acclimatization is indicated by an increase in sweat rate and stoke volume (amount of blood pumped per heartbeat), and a decrease in heart rate, core temperature, skin temperature and sweat salt loss.
One of the best organizations in the world at this process? The United States military. Here are some strategies they recommend:
- Start slowly and reduce work intensity and duration
- Acclimatize in the heat of the day, reserve harder work for the coolest times
- Use work and rest to modify heat strain Ensure four to fourteen days of exposure (depending on environment)
- Maintain daily duration of at least 100 minutes
- When possible, begin process up to one month before work begins
While it all seems simple enough, the challenge with acclimatization is often that workers may not always be thrilled to comply—particularly new members of the crew looking to prove they can pull their weight right off the bat. That’s why it’s important to go beyond merely encouraging it to actually make it a worksite protocol.
HEAT STRESS PREVENTION FACTOR 3:
WORK-TO-REST RATIO
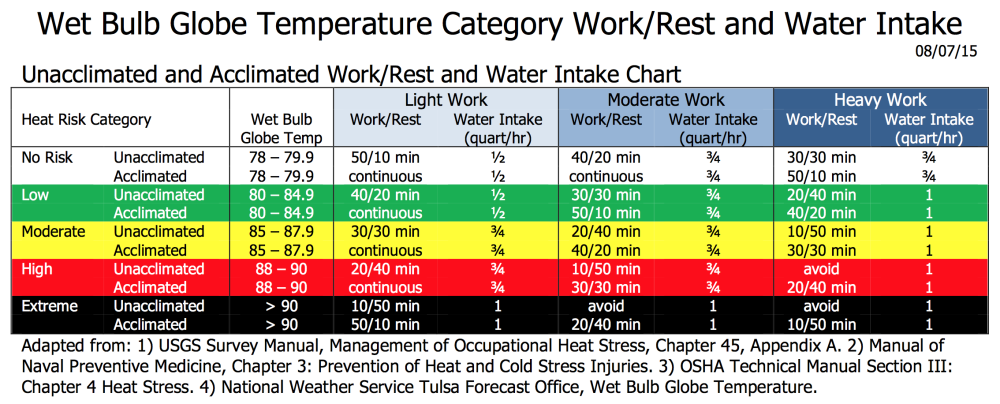
Prevention doesn’t stop at acclimatization. Even those who have been working in extreme heat for many years can be subject to life-altering heat stress illnesses if safety managers aren’t attentive to changing conditions. Once temperatures surpass 75°F, a site’s standard work time to rest time ratio needs to be modified.

When modifying work/break times, there are many variables to consider beyond temperature—including work intensity, time of day, PPE and equipment, even things like individual worker age and health conditions. Safe working conditions for a 22-year-old are likely not the same as those for a 45-year old.
For the most accurate measurement on a site’s conditions, OSHA recommends use of the Wet Bulb Globe Temperature monitor—a specialized device that takes into account temperature, humidity, wind speed, sun angle and cloud cover (they’ve also got a handy calculator that can estimate it for you). Of course, a monitor may not always be 100% accurate or accessible. Regardless of if a Wet Bulb Glove Temperature rating is used or not, safety managers should set work-rest schedules with both caution and common sense.
HEAT STRESS PREVENTION FACTOR 4:
BODY COOLING
The final big ticket item for heat stress prevention is body cooling. A simple but underutilized strategy, there are a variety of body cooling methods that can be hugely impactful on maintaining safe body temperatures and cooling the surface of the skin. These include things such as shade or the use of cooling PPE to accelerate the evaporation process.
Because there’s no one-size-fits-all solution for every worksite, the Korey Stringer Institute came up with a simple acronym to help safety managers determine what they need—LEFT: Location, Efficacy, Feasibility and Timing.
Location
Where is the site located? Is it remote? Do you have access to power? Some cooling PPE requires refrigeration, so those without access should instead use water-activated technologies. Humidity level and airflow can also have an impact on gear performance. Evaporative cooling products work best in environments with lots of airflow and low to moderate humidity levels. Conversely, phase change technologies perform well regardless of environmental conditions—making them a great solution for high humidity and indoor sites.
Efficacy
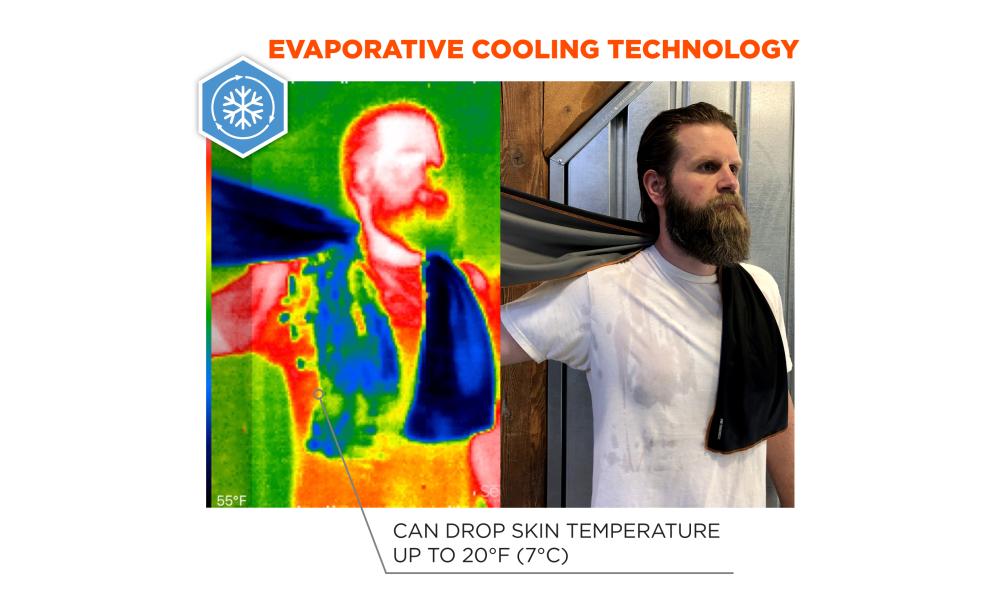
Are the claims made by your “magical” cooling gear substantiated or is it all just smoke and mirrors? Evaporative technologies, for example, work similarly to the body’s natural sweating process by using external water sources to draw heat away. While any damp rag will somewhat deliver the same effect, controlled evaporative gear integrated with microfiber, acrylic polymers or PVA instantly activates to keep workers cool for hours on end.
Feasibility
Can—and will—workers actually use it within the constructs of their job? Are they limited by other PPE requirements? Is utilizing it easy and comfortable or more trouble than it’s worth? For example, workers confined by heavy PPE may have more limited opportunities to drink water. In these instances, cooling PPE they can wear underneath their gear can help keep temperatures a bay.
Timing
Can body cooling solutions be used all the time or just on breaks? Tents and umbrellas are an obvious choice for shading rest areas, but can also be implemented elsewhere on site to relieve workers on the job. When shade isn’t available, cooling PPE designed specifically for wear during work can be hugely beneficial to keeping workers cool throughout the day. This includes solutions such as hard hat liners, towels, sleeves, vests and more.
When it comes to Heat Stress Prevention, OSHA’s Water, Rest and Shade Guidelines are really just the start. While it does lay the groundwork, a complete program goes beyond the basics to also include advanced cooling technologies to keep workers safe both outdoors as well as in. So let’s break down the two main types of cooling PPE and technologies, and talk about how easy they are to use and when and where you would utilize each.
Let’s start with Evaporative Cooling Technology. Evaporative Cooling Technology is going to be ideal for someone working in an environment with adequate airflow and also low-to-moderate humidity levels. To activate an Evaporative Cooling Product, you are going to want to fully saturate the product in water and then expose it to airflow. It’s that easy. Once activated, you’re going to get up to four hours of cooling with that product.
Evaporative Cooling Products come in a variety of different models and styles. You can find them in vest form to help regulate your core body temperature even better or you can find it in accessories—whether that be cooling bandanas, cooling towels or hard hat attachment accessories.
There’s one additional type of Evaporative Cooling Technology that I wanted to touch on and that’s Dry Evaporative Technology. Dry Evaporative Cooling Technology is different from Wet Evaporative in that the wearer stays dry 100% of the time. Just as easy to activate by filling the vest with water, and then you’re going to get up to three days of cooling with that cooling technology.
Moving on to Phase Change… We know it’s not a one-size-fits-all approach and there are workers in a variety of different environments. Those who are working in high heat environments like manufacturing, foundries and bakeries, to name a few, or those who are wearing layers of PPE and do not have access to airflow are going to benefit from a Phase Change Cooling Technology. What’s great about Phase Change is, regardless of environmental variables, once activated, it’s going to stay cool for between two and four hours.
Now, Phase Change packs are easy to activate. Your simply soak them in a bucket of ice water, put them in the refrigerator or a cooler for up to 15 minutes. And as I said, once activated, you don’t have to worry about humidity or airflow. You can wear it under your PPE and you’re going to stay cool for 2 to 4 hours.
For more information on Cooling PPE and Heat Stress Basic Awareness, search Heat Stress on our Tenacious Blog at Ergodyne.com
BONUS FACTOR! EDUCATION
If we really want to reduce the risk, we also need to change the culture. One of the best defenses against the “toughing out out” mindset is continuing to educate crews on just how deadly serious heat stress can be. Learn more common heat stress illnesses and solutions you can implement today to prevent them in our comprehensive guide.